Acute aortic syndrome
| Acute aortic syndrome | |
|---|---|
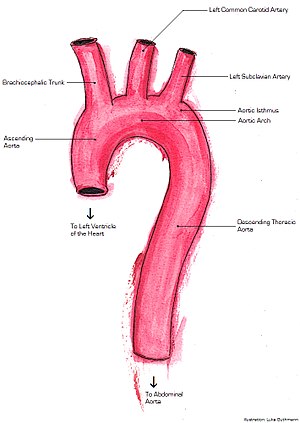 | |
| Major aorta anatomy displaying ascending aorta, brachiocephalic trunk, left common carotid artery, left subclavian artery, aortic isthmus, aortic arch, and descending thoracic aorta | |
| Specialty | Vascular surgery |
Acute aortic syndrome (AAS) describes a range of severe, painful, potentially life-threatening abnormalities of the aorta.[1] These include aortic dissection, intramural thrombus, and penetrating atherosclerotic aortic ulcer.[2] AAS can be caused by a lesion on the wall of the aorta that involves the tunica media, often in the descending aorta.[3] It is possible for AAS to lead to acute coronary syndrome.[4] The term was introduced in 2001.[5][6]
Signs and symptoms
The most common symptom of AAS is sudden and severe chest pain. However, other variants of chest pain and back pain have been described.[7]
Causes
Causes can include aortic dissection (which is the most common type),[8] intramural hematoma, penetrating atherosclerotic ulcer or a thoracic aneurysm that has become unstable.[9] The potential causes of AAS are life-threatening and present with similar symptoms, making it difficult to distinguish the ultimate cause, though high resolution, high contrast computerised tomography can be used.[9][10]
Diagnosis
The condition can be mimicked by a ruptured cyst of the pericardium,[11] ruptured aortic aneurysm[10] and acute coronary syndrome.[12]
Misdiagnosis is estimated at 39% and is associated with delays correct diagnosis and improper treatment with anticoagulants producing excessive bleeding and extended hospital stays.[12]
Management
AAS is life-threatening, with a high mortality rate if appearing acutely, reduced only when diagnosed early and treated by a surgeon with considerable expertise.[3] If patients survive acute presentation, within three to five years 30% will develop complications and require close follow-up.[3] Early diagnosis is essential for survival and management is challenging though greater awareness of the syndrome and improving management strategies are improving patient outcomes.[13]
References
- ^ Ahmad F, Cheshire N, Hamady M (May 2006). "Acute aortic syndrome: pathology and therapeutic strategies". Postgrad Med J. 82 (967): 305–12. doi:10.1136/pgmj.2005.043083. PMC 2563796. PMID 16679467.
- ^ Macura, KJ; Corl FM; Fishman EK; Bluemke DA (1 August 2003). "Pathogenesis in acute aortic syndromes: aortic dissection, intramural hematoma, and penetrating atherosclerotic aortic ulcer". American Journal of Roentgenology. 181 (2): 309–316. doi:10.2214/ajr.181.2.1810309. PMID 12876003.
- ^ a b c Evangelista Masip A (April 2007). "[Progress in the acute aortic syndrome]". Rev Esp Cardiol (in Spanish). 60 (4): 428–39. doi:10.1157/13101646. PMID 17521551.
- ^ Manghat NE, Morgan-Hughes GJ, Roobottom CA (December 2005). "Multi-detector row computed tomography: imaging in acute aortic syndrome". Clin Radiol. 60 (12): 1256–67. doi:10.1016/j.crad.2005.06.011. PMID 16291307.
- ^ van der Loo B, Jenni R (August 2003). "Acute aortic syndrome: proposal for a novel classification". Heart. 89 (8): 928. doi:10.1136/heart.89.8.928. PMC 1767786. PMID 12860875.
- ^ Vilacosta I, Román JA (April 2001). "Acute aortic syndrome". Heart. 85 (4): 365–8. doi:10.1136/heart.85.4.365. PMC 1729697. PMID 11250953.
- ^ Murphy, Michael C.; Castner, Catherine F.; Kouchoukos, Nicholas T. (2017). "Acute Aortic Syndromes: Diagnosis and Treatment". Missouri Medicine. 114 (6): 458–463. ISSN 0026-6620. PMC 6139964. PMID 30228665.
- ^ Gregory, Stephen H.; Yalamuri, Suraj M.; Bishawi, Muath; Swaminathan, Madhav (December 2018). "The Perioperative Management of Ascending Aortic Dissection". Anesthesia & Analgesia. 127 (6): 1302–1313. doi:10.1213/ANE.0000000000003747. ISSN 0003-2999. PMID 30211773. S2CID 52195386.
- ^ a b Smith AD, Schoenhagen P (January 2008). "CT imaging for acute aortic syndrome". Cleve Clin J Med. 75 (1): 7–9, 12, 15–7 passim. doi:10.3949/ccjm.75.1.7. PMID 18236724.
- ^ a b Marijon E, Vilanculos A, Tivane A, et al. (2007). "Thoracic aortic aneurysm: direct sign of rupture". Cardiovasc J Afr. 18 (3): 180–1. PMID 17612751.
- ^ Nishigami K, Hirayama T, Kamio T (February 2008). "Pericardial cyst rupture mimicking acute aortic syndrome". Eur. Heart J. 29 (14): 1752. doi:10.1093/eurheartj/ehn038. PMID 18296680.
- ^ a b Hansen MS, Nogareda GJ, Hutchison SJ (March 2007). "Frequency of and inappropriate treatment of misdiagnosis of acute aortic dissection". Am. J. Cardiol. 99 (6): 852–6. doi:10.1016/j.amjcard.2006.10.055. PMID 17350381.
- ^ Ince H, Nienaber CA (May 2007). "[Management of acute aortic syndromes]". Rev Esp Cardiol (in Spanish). 60 (5): 526–41. doi:10.1016/S1885-5857(07)60194-7. PMID 17535765.