Platelet_factor_4
Platelet factor 4 (PF4) is a small cytokine belonging to the CXC chemokine family that is also known as chemokine (C-X-C motif) ligand 4 (CXCL4) . This chemokine is released from alpha-granules of activated platelets during platelet aggregation, and promotes blood coagulation by moderating the effects of heparin-like molecules. Due to these roles, it is predicted to play a role in wound repair and inflammation.[5] It is usually found in a complex with proteoglycan.
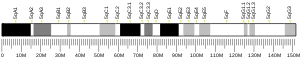
Genomics
The gene for human PF4 is located on human chromosome 4.[6]
Function
Platelet factor-4 is a 70-amino acid protein that is released from the alpha-granules of activated platelets and binds with high affinity to heparin. Its major physiologic role appears to be neutralization of heparin-like molecules on the endothelial surface of blood vessels, thereby inhibiting local antithrombin activity and promoting coagulation. As a strong chemoattractant for neutrophils and fibroblasts, PF4 probably has a role in inflammation and wound repair.[5][7]
PF4 is chemotactic for neutrophils, fibroblasts and monocytes, and interacts with a splice variant of the chemokine receptor CXCR3, known as CXCR3-B.[8]
Clinical significance
The heparin:PF4 complex is the antigen in heparin-induced thrombocytopenia (HIT), an idiosyncratic autoimmune reaction to the administration of the anticoagulant heparin.[9] PF4 autoantibodies have also been found in patients with thrombosis and features resembling HIT but no prior administration of heparin.[10] Antibodies against PF4 have been implicated in cases of thrombosis and thrombocytopenia subsequent to vaccination with the Oxford–AstraZeneca or the Janssen COVID-19 vaccine.[11][12] This phenomenon has been termed vaccine-induced immune thrombotic thrombocytopenia (VITT).[13] Changes in the expression of PF4 have also been associated with symptoms of long COVID.[14]
It is increased in patients with systemic sclerosis that also have interstitial lung disease.[15]
The human platelet factor 4 kills malaria parasites within erythrocytes by selectively lysing the parasite's digestive vacuole.[16]
See also
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000163737 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000029373 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Eisman R, Surrey S, Ramachandran B, Schwartz E, Poncz M (July 1990). "Structural and functional comparison of the genes for human platelet factor 4 and PF4alt". Blood. 76 (2): 336–44. doi:10.1182/blood.V76.2.336.336. PMID 1695112.
- ^ O'Donovan N, Galvin M, Morgan JG (1999). "Physical mapping of the CXC chemokine locus on human chromosome 4". Cytogenetics and Cell Genetics. 84 (1–2): 39–42. doi:10.1159/000015209. PMID 10343098. S2CID 8087808.
- ^ "Entrez Gene: PF4 platelet factor 4 (chemokine (C-X-C motif) ligand 4)".
- ^ Lasagni L, Francalanci M, Annunziato F, Lazzeri E, Giannini S, Cosmi L, et al. (June 2003). "An alternatively spliced variant of CXCR3 mediates the inhibition of endothelial cell growth induced by IP-10, Mig, and I-TAC, and acts as functional receptor for platelet factor 4". The Journal of Experimental Medicine. 197 (11): 1537–49. doi:10.1084/jem.20021897. PMC 2193908. PMID 12782716.
- ^ Warkentin TE (March 2007). "Drug-induced immune-mediated thrombocytopenia--from purpura to thrombosis". The New England Journal of Medicine. 356 (9): 891–3. doi:10.1056/NEJMp068309. PMID 17329695.
- ^ Warkentin TE, Makris M, Jay RM, Kelton JG (July 2008). "A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia". The American Journal of Medicine. 121 (7): 632–6. doi:10.1016/j.amjmed.2008.03.012. PMID 18589060.
- ^ Schultz NH, Sørvoll IH, Michelsen AE, Munthe LA, Lund-Johansen F, Ahlen MT, et al. (April 2021). "Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination". The New England Journal of Medicine. 384 (22): 2124–2130. doi:10.1056/NEJMoa2104882. ISSN 0028-4793. PMC 8112568. PMID 33835768.
- ^ Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S (April 2021). "Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination". The New England Journal of Medicine. 384 (22): 2092–2101. doi:10.1056/NEJMoa2104840. PMC 8095372. PMID 33835769.
- ^ Arepally GM, Ortel TL (June 2021). "Vaccine-Induced Immune Thrombotic Thrombocytopenia (VITT): What We Know and Don't Know". Blood. doi:10.1182/blood.2021012152. PMC 8172307. PMID 34061166.
- ^ Ryan FJ, Hope CM, Masavuli MG, Lynn MA, Mekonnen ZA, Yeow AE, et al. (January 2022). "Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection". BMC Medicine. 20 (1): 26. doi:10.1186/s12916-021-02228-6. PMC 8758383. PMID 35027067.
- ^ Volkmann ER, Tashkin DP, Roth MD, Clements PJ, Khanna D, Furst DE, et al. (December 2016). "Changes in plasma CXCL4 levels are associated with improvements in lung function in patients receiving immunosuppressive therapy for systemic sclerosis-related interstitial lung disease". Arthritis Research & Therapy. 18 (1): 305. doi:10.1186/s13075-016-1203-y. PMC 5203703. PMID 28038680.
- ^ Love MS, Millholland MG, Mishra S, Kulkarni S, Freeman KB, Pan W, et al. (December 2012). "Platelet factor 4 activity against P. falciparum and its translation to nonpeptidic mimics as antimalarials". Cell Host & Microbe. 12 (6): 815–23. doi:10.1016/j.chom.2012.10.017. PMC 3638032. PMID 23245326.
Further reading
- Bikfalvi A, Gimenez-Gallego G (February 2004). "The control of angiogenesis and tumor invasion by platelet factor-4 and platelet factor-4-derived molecules". Seminars in Thrombosis and Hemostasis. 30 (1): 137–44. doi:10.1055/s-2004-822978. PMID 15034805. S2CID 260320397.
- Maurer AM, Zhou B, Han ZC (December 2006). "Roles of platelet factor 4 in hematopoiesis and angiogenesis". Growth Factors. 24 (4): 242–52. doi:10.1080/08977190600988225. PMID 17381065. S2CID 36468865.
- Deuel TF, Keim PS, Farmer M, Heinrikson RL (June 1977). "Amino acid sequence of human platelet factor 4". Proceedings of the National Academy of Sciences of the United States of America. 74 (6): 2256–8. Bibcode:1977PNAS...74.2256D. doi:10.1073/pnas.74.6.2256. PMC 432148. PMID 267922.
- Walz DA, Wu VY, de Lamo R, Dene H, McCoy LE (December 1977). "Primary structure of human platelet factor 4". Thrombosis Research. 11 (6): 893–8. doi:10.1016/0049-3848(77)90117-7. PMID 601757.
- Nath N, Lowery CT, Niewiarowski S (April 1975). "Antigenic and antiheparin properties of human platelet factor 4 (PF4)". Blood. 45 (4): 537–50. doi:10.1182/blood.V45.4.537.537. PMID 803847.
- Hermodson M, Schmer G, Kurachi K (September 1977). "Isolation, crystallization, and primary amino acid sequence of human platelet factor 4". The Journal of Biological Chemistry. 252 (18): 6276–9. doi:10.1016/S0021-9258(17)39951-9. PMID 893407.
- Maione TE, Gray GS, Petro J, Hunt AJ, Donner AL, Bauer SI, et al. (January 1990). "Inhibition of angiogenesis by recombinant human platelet factor-4 and related peptides". Science. 247 (4938): 77–9. Bibcode:1990Sci...247...77M. doi:10.1126/science.1688470. PMID 1688470.
- Han ZC, Bellucci S, Tenza D, Caen JP (April 1990). "Negative regulation of human megakaryocytopoiesis by human platelet factor 4 and beta thromboglobulin: comparative analysis in bone marrow cultures from normal individuals and patients with essential thrombocythaemia and immune thrombocytopenic purpura". British Journal of Haematology. 74 (4): 395–401. doi:10.1111/j.1365-2141.1990.tb06325.x. PMID 2140694. S2CID 24529258.
- Poncz M, Surrey S, LaRocco P, Weiss MJ, Rappaport EF, Conway TM, Schwartz E (January 1987). "Cloning and characterization of platelet factor 4 cDNA derived from a human erythroleukemic cell line". Blood. 69 (1): 219–23. doi:10.1182/blood.V69.1.219.219. PMID 3098319.
- Griffin CA, Emanuel BS, LaRocco P, Schwartz E, Poncz M (1987). "Human platelet factor 4 gene is mapped to 4q12----q21". Cytogenetics and Cell Genetics. 45 (2): 67–9. doi:10.1159/000132431. PMID 3622011.
- Senior RM, Griffin GL, Huang JS, Walz DA, Deuel TF (February 1983). "Chemotactic activity of platelet alpha granule proteins for fibroblasts". The Journal of Cell Biology. 96 (2): 382–5. doi:10.1083/jcb.96.2.382. PMC 2112304. PMID 6187750.
- Morgan FJ, Begg GS, Chesterman CN (February 1980). "Complete covalent structure of human platelet factor 4". Thrombosis and Haemostasis. 42 (5): 1652–60. PMID 6445090.
- Deuel TF, Senior RM, Chang D, Griffin GL, Heinrikson RL, Kaiser ET (July 1981). "Platelet factor 4 is chemotactic for neutrophils and monocytes". Proceedings of the National Academy of Sciences of the United States of America. 78 (7): 4584–7. Bibcode:1981PNAS...78.4584D. doi:10.1073/pnas.78.7.4584. PMC 319837. PMID 6945600.
- Brown KJ, Parish CR (November 1994). "Histidine-rich glycoprotein and platelet factor 4 mask heparan sulfate proteoglycans recognized by acidic and basic fibroblast growth factor". Biochemistry. 33 (46): 13918–27. doi:10.1021/bi00250a047. PMID 7524669.
- Mayo KH, Roongta V, Ilyina E, Milius R, Barker S, Quinlan C, et al. (September 1995). "NMR solution structure of the 32-kDa platelet factor 4 ELR-motif N-terminal chimera: a symmetric tetramer". Biochemistry. 34 (36): 11399–409. doi:10.1021/bi00036a012. PMID 7547867.
- Barker S, Mayo KH (January 1995). "Quarternary structure amplification of protein folding differences observed in 'native' platelet factor-4". FEBS Letters. 357 (3): 301–4. Bibcode:1995FEBSL.357..301B. doi:10.1016/0014-5793(94)01384-D. PMID 7835432. S2CID 12222261.
- Zhang X, Chen L, Bancroft DP, Lai CK, Maione TE (July 1994). "Crystal structure of recombinant human platelet factor 4". Biochemistry. 33 (27): 8361–6. doi:10.1021/bi00193a025. PMID 8031770.
- Horne MK (April 1993). "The effect of secreted heparin-binding proteins on heparin binding to platelets". Thrombosis Research. 70 (1): 91–8. doi:10.1016/0049-3848(93)90226-E. PMID 8511754.
- Kolset SO, Mann DM, Uhlin-Hansen L, Winberg JO, Ruoslahti E (April 1996). "Serglycin-binding proteins in activated macrophages and platelets". Journal of Leukocyte Biology. 59 (4): 545–54. doi:10.1002/jlb.59.4.545. PMID 8613703. S2CID 23125881.
External links
- Platelet+factor+4 at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.